Rocky Mountain Spotted Fever: Symptoms, Causes, and Treatment Options

Although many Americans are looking forward to warmer months, spring and summer are seasons when various tick-borne illnesses become more prevalent.
One such disease is Rocky Mountain spotted fever (RMSF) – a condition that can cause severe complications if left untreated.
In this article, we’ll look at everything you need to know about identifying RMSF, seeking treatment, and preventing recurrent infections for a tick-free summer.
What is Rocky Mountain Spotted Fever?
Rocky Mountain spotted fever (RMSF) is a severe infectious disease caused by the bite of a tick carrying the Rickettsia rickettsii bacteria.
The disease is primarily transmitted by the American dog tick, Rocky Mountain wood tick, and brown dog tick commonly found in the Rocky Mountains and Pacific Coast.
RMSF is most prevalent in the spring and early summer, when outdoor activities increase your risk of tick exposure.
Signs and symptoms
The symptoms of RMSF typically begin two to 14 days after being bitten by an infected tick.
Recognizing these symptoms early on is crucial as the disease progresses rapidly and may cause potentially life-threatening symptoms.
Early symptoms of RMSF may include:
- A sudden, high fever between 102°F to 104°F
- Severe headaches that typically occur in the forehead, temples, or the back of the neck
- Deep muscle pain
- Gastrointestinal symptoms, such as nausea, vomiting, abdominal pain, and diarrhea
- Sudden onset of a rash
If you delay getting treatment for RMSF, you may develop more severe symptoms that indicate an advanced infection. These symptoms include:
- Confusion or an altered mental state
- Shortness of breath
- Seizures
- Numbness or weakness
- Anxiety, nervousness, or agitation
Key Point: What Does an RMSF Rash Look Like?
A RMSF rash usually develops within five days of infection and it is one of the most obvious signs of this disease.
This rash may appear as small, flat, pink spots on the wrists, forearms, and ankles. As it develops, it can spread to the neck, chest, back, legs, and soles of the feet.
Over time, the rash may become raised and turn a reddish-purple color. This usually only happens in severe RMSF infections.
Causes of Rocky Mountain Spotted Fever
RMSF is primarily transmitted through infected tick bites. These ticks become carriers of the disease by feeding on infected animals, such as rodents or small mammals.
Infected ticks can transmit the RSMF virus to humans. The tick needs to be attached to your skin for at least four to six hours before the bacteria can be transmitted.
However, tick bites are often painless, so many people don’t notice the insect quickly enough to remove it before it can transmit the disease.
If you do notice a tick or tick bites on your body, seek emergency medical care as soon as possible to ensure prompt treatment.
How is RMSF Diagnosed?
Your doctor will use a combination of clinical assessments and laboratory tests to diagnose RSMF. Early diagnosis and treatment are crucial to prevent severe complications.
During the diagnostic process, your healthcare provider may follow these steps:
-
Symptom evaluation: The first step in diagnosing RMSF is the evaluation of symptoms. Doctors will look for the classic signs of RMSF — such as a sudden high fever, severe headache, muscle pain, and the characteristic rash — that may develop a few days after infection.
-
Patient history: Providing a detailed history of your recent activities is crucial, especially if tick exposure is suspected. Knowing if you have been in tick-infested areas can help your doctor make an accurate diagnosis.
Depending on the results of these evaluations, your doctor may recommend further testing that could include:
-
Polymerase chain reaction (PCR) testing: A PCR test can detect RMSF bacteria DNA in a blood sample or skin biopsy taken from the rash site. This test is used for early detection and is typically the first choice to confirm an RMSF diagnosis.
-
Skin biopsy: A tissue sample from the rash can be examined under a microscope using immunohistochemistry (HC) staining to detect Rickettsia species.
-
Serological tests: These tests detect antibodies that develop against RMSF bacteria. However, antibodies may not be detectable in the first week of infection, which can complicate early diagnosis.
Once you’ve been diagnosed with RMSF, your doctor will recommend an appropriate treatment regime to help you overcome the infection and avoid serious complications.
What are the Treatment Options for RMSF?
Antibiotics
Antibiotics are usually the first-line treatment for RMSF and can be given to infected people of all ages, including children.
Doxycycline is the preferred antibiotic and is often administered within the first five days of showing symptoms.
It targets RMSF-causing bacteria and inhibits the organisms’ growth to prevent the disease from becoming more severe.
This way, doxycycline can effectively help reduce the risk of developing severe and potentially fatal complications.
Chloramphenicol is an alternative to doxycycline and may be used when individuals are allergic to the primary antibiotic.
However, chloramphenicol typically has more severe side effects than doxycycline and may also be less effective.
Blood transfusion
In severe cases of RMSF, individuals may develop significant health complications — such as anemia or thrombocytopenia — that can cause spontaneous bleeding.
These conditions may require blood transfusions to manage them and stabilize the individual.
Mechanical ventilation
If RMSF spreads or worsens, it can cause acute respiratory distress and other breathing complications.
Individuals who experience significant respiratory issues may require mechanical ventilation to support their breathing while antibiotics are used to treat RMSF.
Potential Complications of RMSF
Even with treatment, RMSF can cause potentially life-threatening complications. These may include:
- Acute respiratory distress syndrome (ARDS)
- Pulmonary edema
- Acute kidney injury (AKI)
- Anemia
- Heart disease
- Internal bleeding
- Partial paralysis
- Sepsis
- Fecal incontinence or urinary incontinence
- Gangrene that may require amputation
- Organ failure
- Inflammation of the brain (encephalitis)
Individuals who are severely ill from RMSF may also develop long-term health issues, including:
- Nerve damage
- Paralysis
- Speech difficulties
- Hearing loss
- Vision loss
- Neurological difficulties, like vertigo
To prevent these complications, seek prompt medical treatment. If you develop any symptoms of RMSF, consult your doctor as soon as possible.
Can You Prevent RMSF?
Preventing RMSF involves using strategies to avoid tick exposure and bites. These strategies may include:
-
Using an insect repellent that contains DEET, picaridin, or IR3535 on exposed skin and clothing
-
Wearing protective clothing — such as long-sleeved shirts, long pants, and hats — to prevent ticks from getting to the skin
-
Choosing light-colored clothing that makes it easier to spot ticks before they reach the skin
-
Avoiding home remedies like using nail polish or petroleum jelly to remove a tick as these may not be effective and increase your infection risk
-
Using fine-tipped tweezers to remove the tick promptly
-
Showering within two hours of coming indoors to wash off unwanted ticks and reduce your risk of infection
-
Performing regular and thorough tick checks, especially when you’ve spent time outdoors
-
Using landscaping to create barriers between wooded areas and your yard to establish tick-free zones — especially in tick-infested habitats
These strategies can help you reduce your risk of exposure to infectious ticks and minimize your chances of getting diseases like RMSF.
When Should You See a Doctor About RMSF?
RMSF is a serious disease that requires immediate medical attention as soon as it’s suspected.
If not promptly treated, the disease can rapidly progress, causing potentially life-threatening complications.
You should consult your doctor immediately if you experience any of the following:
-
Known signs of RMSF infection including severe headaches, muscle pain, fever, and general malaise
-
A rash that appears as flat, pink spots on the arms, legs, ankles, and soles of the feet
-
Unexplained gastrointestinal symptoms
-
Respiratory issues
-
Neurological issues, including confusion and coordination difficulties
Even without these symptoms, you should see your doctor if you discover a tick bite anywhere on your body.
Although it may not be an RMSF-infected tick, many similar diseases can develop from a bite — including Lyme disease.
Seeking immediate medical care can help you get prompt treatment and avoid the complications associated with tick-borne illnesses.
Where Can You Learn More About RMSF?
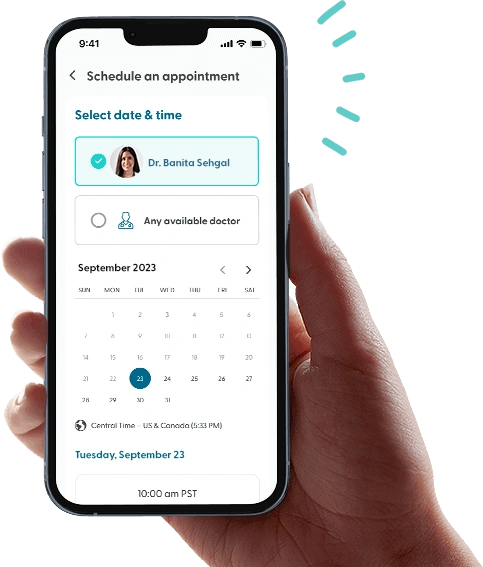
While LifeMD doesn’t provide medical care for RMSF, we can help you manage any unpleasant symptoms you may be experiencing.
A team of medical professionals can assist you with medications, prescriptions, and advice to cope with painful or uncomfortable symptoms caused by an infected tick bite.
Make your appointment and take control of your health — all from the comfort of your own home.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD today and experience amazing healthcare, discounted labs and prescription medications... plus around-the-clock access to medical guidance.