A Comprehensive Overview of Tick-Borne Encephalitis
According to the Centers for Disease Control and Prevention (CDC), up to 10,000 cases of tick-borne encephalitis (TBE) occur globally each year.
Flu-like symptoms typically accompany this disease and pass within five days.
However, some people might develop a more severe form of the disease, which is why it’s important to seek medical treatment as soon as you suspect you have TBE.
In this article, we’ll provide insights into tick-borne encephalitis and its symptoms to help you determine if you should be concerned about this condition.
What is Tick-Borne Encephalitis (TBE)?
Like other tick-borne diseases, tick-borne encephalitis (TBE) is a virus caused by tick bites. The infected tick transmits the TBE virus to a human through its bite.
While ticks are the primary carriers of this virus, other animals, including rodents, deer, sheep, and goats, may also carry TBE.
Although ticks can spread the virus to humans, it can’t be passed from one person to another.
In rare cases, humans have been infected with the TBE virus by drinking unpasteurized milk from goats, sheep, and cows.
Where Can I Get Tick-Borne Encephalitis?
There are certain parts of the world where the TBE virus is more common. These are known as endemic areas.
The endemic regions for tick-borne encephalitis include parts of Europe, such as:
Estonia
Slovenia
Latvia
Lithuania
Czechia
Austria
Sweden
Switzerland
Slovakia
Hungary
Poland
Finland
Germany
France
Croatia
Norway
Other endemic areas include Siberia, Far Eastern Russia, Northern China, and Japan. In recent years, the tick-borne encephalitis virus has also been found in the Netherlands and the UK.
The risk of contracting tick-borne encephalitis virus is highest in spring, summer, and early fall, which is when the ticks that spread the disease are most active.
If you feel ill after traveling to an endemic area during peak tick seasons, seek medical attention as there’s a possibility you may have contracted the TBE virus.
The Initial Symptoms of Tick-Borne Encephalitis
Most people infected with the TBE virus won’t show any symptoms. Those who do have symptoms will probably experience them for around five days.
The incubation period for TBE is seven to 14 days. This means you may not have symptoms immediately after being bitten by a tick.
The symptoms of the initial phase of the TBE virus include:
Fever
When a tick transmits the TBE virus to a human, the body identifies it as a foreign invader. This triggers the immune system, which responds by raising the body's temperature as one of its initial defenses.
Aches
The TBE virus triggers an inflammatory response within the body, during which chemicals called cytokines and chemokines are released to fight the virus.
Although they help the body, these chemicals can stimulate nerve endings, leading to joint pain and muscle aches.
Loss of appetite
Some cytokines impact a part of the brain called the hypothalamus, which controls appetite. The changes in levels of cytokines in the body can suppress the appetite while the body prioritizes fighting the virus.
The infection may also make individuals feel sick and fatigued. This can decrease your desire to eat.
Headaches
This tick-borne virus primarily affects the central nervous system (CNS), which includes the brain and its surrounding protective layers — known as the meninges.
The virus may lead to inflammation in the meninges, which increases the pressure inside the skull and causes headaches.
Cytokines can also contribute to swelling and inflammation in the brain, which can worsen headaches.
Nausea and vomiting
As the TBE virus can impact the brain, it may affect the areas of the organ that regulate nausea and vomiting. These areas can become inflamed or irritated by the infection, which can trigger nausea and vomiting.
The release of cytokines and other inflammatory chemicals to help fight the infection can also activate the brain regions that control nausea and vomiting.
Risk Factors for Tick-Borne Encephalitis
Certain people have a higher risk of developing the TBE virus. Risk factors include:
Geographical location: If you live in or are going to visit an endemic area, you have a higher risk of contracting the TBE virus. This is especially true if you spend time in forested areas, grassland, or places with underbrush and high grass.
Outdoor activities: If you engage in activities such as hiking, camping, fishing, or hunting in areas where there are infected ticks, your risk of being bitten increases.
Age: While TBE can affect any age group, older adults may experience more severe forms of the disease, especially in the second phase.
A weakened immune system: Individuals with compromised immune systems due to medical conditions or medications may be at higher risk for severe disease.
Understanding the Second Phase of Tick-Borne Encephalitis
Some people — especially those with a higher risk of developing TBE because of age or a weakened immune system — may experience the second phase of the virus.
The second phase starts after an approximate two-week period with no symptoms after the initial infection. This second phase of the illness may affect the brain, nerves, or both.
This phase of the TBE virus impacts the central nervous system, and high-risk patients may develop meningitis or encephalitis, which is inflammation of the lining of the brain.
Symptoms of encephalitis and meningitis that patients may experience include:
Neck stiffness
Headaches
Nausea
Impaired consciousness
Poor coordination
Tremors
Personality changes
Psychosis
Muscle pain
Muscle weakness, often in the arms
In some cases, the TBE virus may affect the muscles that control breathing, which can be fatal.
The severity of the second phase varies among individuals — some may only have a mild illness, while others may experience severe symptoms.
How is Tick-Borne Encephalitis Diagnosed?
The TBE virus is usually diagnosed by testing a sample of your blood. This will help your healthcare provider detect the first phase of the illness.
If you suspect you have the second phase of the TBE virus, you may need a lumbar puncture (LP) — sometimes called a spinal tap — for diagnosis.
This procedure involves inserting a needle into the base of the spine to collect cerebrospinal fluid — the fluid that surrounds the brain and spinal cord — for testing.
Treatment for Tick-Borne Encephalitis
There is no specific treatment designed for tick-borne encephalitis. Healthcare professionals typically prescribe treatments for symptom management, such as pain relievers.
This is because most individuals only need to control their symptoms temporarily until they recover.
Individuals with severe disease may require hospitalization for supportive care.
Supportive treatment may include help with breathing, hydration, and reducing brain swelling, particularly if they develop meningitis or encephalitis.
The Long-Term Implications of Tick-Borne Encephalitis
While most people with tick-borne encephalitis will recover completely, high-risk individuals may experience long-term effects from the virus that include:
Paralysis: The inability to move the arms or legs
Ataxia: Difficulties with balance, speech, coordination, and communication
People with long-term side effects may also experience:
Headaches
Fatigue
Concentration difficulties
Poor memory
If children contract the TBE virus, they may also have side effects for extended periods, including cognitive problems. This may involve short-term memory issues, fatigue, and irritability.
Getting the Tick-Borne Encephalitis Vaccine
People who plan on moving to TBE-endemic areas and will be exposed to ticks are advised to get a tick-borne encephalitis vaccine.
If you’ll be traveling to a TBE-endemic region and may be engaging in outdoor activities where ticks are likely to be found, the vaccine is also recommended.
Your healthcare provider will assess your need for the vaccine based on whether you’re at risk of a tick bite and developing the tick-borne encephalitis virus.
Aside from getting the vaccine, knowing where to expect ticks and taking steps to prevent tick bites in these areas is important.
Where Can I Learn More About Tick-Borne Encephalitis?
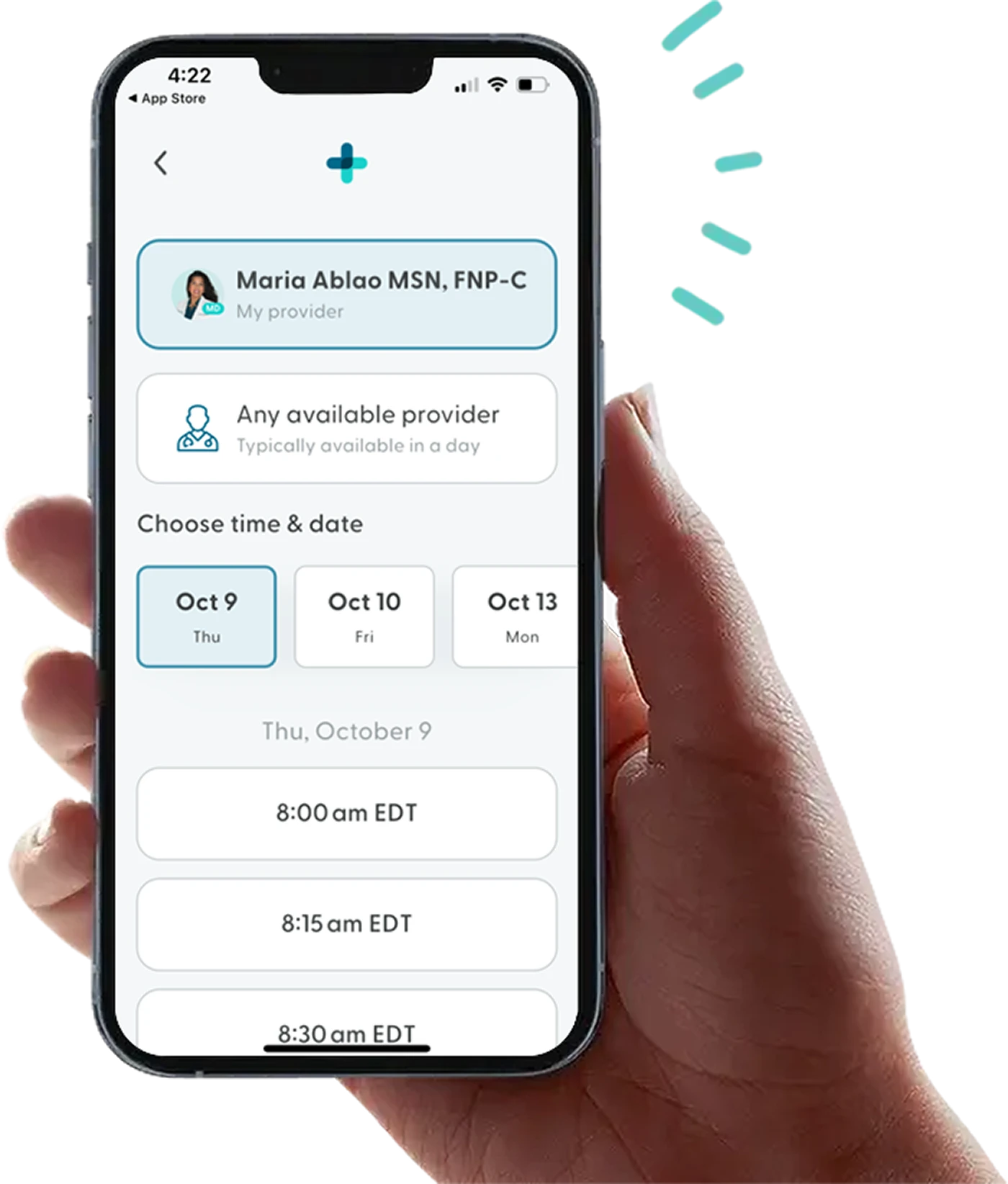
If you have the TBE virus and you’re experiencing uncomfortable or unpleasant symptoms, LifeMD can help.
While we can’t treat tick-borne encephalitis specifically, we can help manage your symptoms and provide advice to help you recover.
A team of medical professionals can assist you with medications, prescriptions, and advice to cope with painful or uncomfortable symptoms caused by an infected tick bite.
Make your appointment today to take control of your health — all from the comfort of your own home.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.