From Field to Infection: A Closer Look at Tularemia Symptoms and Treatments
As the summer hunting season approaches, many Americans may find themselves at an increased risk of contracting infectious diseases, such as tularemia.
Although rare, tularemia is a serious infection. Understanding the risk factors and symptoms can help protect your health.
In this article, we’ll look at everything you need to know about tularemia, including when to seek treatment and what you can do to reduce your infection risk.
What is Tularemia?
Tularemia — commonly known as rabbit fever — is a rare infectious disease that primarily affects wild rodents, hares, and rabbits.
It’s caused by the bacteria Francisella tularensis and is typically quite severe.
In fact, tularemia is considered a significant public health concern and is even recognized as a potential form of bioterrorism, which involves the intentional release of harmful biological agents to sicken crops, livestock, and even people.
Humans can contract this disease through direct contact with infected animals or insects.
Symptoms of tularemia
Symptoms of tularemia can vary, depending on the route of the infection. Most symptoms appear within three to five days of exposure and may include:
Fever
Chills
Headaches
Ulcers at infection sites
Swollen and painful lymph glands
Eye irritation or inflammation
Sore throat
Mouth ulcers
Tonsillitis
Cough
Chest pain
In severe cases of tularemia, individuals may experience high fever, fatigue, vomiting, diarrhea, and difficulty breathing.
What Causes Tularemia?
Contact with infected animals
One of the most common causes of tularemia is direct contact with infected animals – especially wild rabbits, hares, and rodents.
This is why tularemia usually affects hunters and individuals involved in skinning or handling carcasses of infected animals, putting them at a higher risk of contracting tularemia.
The bacteria can enter the body through cuts or abrasions in the skin — causing glandular tularemia — or through mucous membranes, leading to infection.
Bites from infected insects
Another common cause of tularemia is bites from infected insects like ticks and flies.
When these insects feed on infected animals and then bite a human, they can transmit the tularemia bacteria into a person’s bloodstream.
Inhaling contaminated aerosols
Inhaling aerosols contaminated with Francisella tularensis is a less common but more dangerous route of transmission.
This infection can occur by distributing contaminated soil, handling infected hay, straw, or grain, or through agricultural and landscaping activities.
Infection through aerosols is particularly concerning because it can lead to pneumonic tularemia, the most severe form of the disease.
Consuming contaminated food or water
This route of transmission may involve drinking untreated water from a natural source where an infected animal has died or where runoff from infected soil has occurred.
Infection through drinking contaminated water can lead to oropharyngeal tularemia, causing symptoms in the mouth and throat.
You can also become infected by consuming contaminated food, such as eating meat from an infected animal.
How is Tularemia Diagnosed?
Diagnosing tularemia can be tricky because it’s such a rare disease. It also shares symptoms with many other conditions, so it can be challenging to identify.
Your doctor may use the following approach to provide an accurate diagnosis:
Clinical evaluation: The first step in diagnosing tularemia involves your doctor reviewing your symptoms and medical history. Your doctor will enquire about your potential exposure to the disease, such as recent tick bites or contact with wild animals.
Laboratory tests: After your clinical evaluation, your doctor may order lab tests. This may include blood tests and checking for antibodies.
In some cases — such as when pneumonia is suspected — your doctor may request imaging tests, like X-rays or CT scans.
Once your diagnosis has been confirmed, your doctor will recommend appropriate treatment options.
Key Point: Risk Factors for Tularemia
While anyone can be infected with tularemia, certain groups of people are more at risk. This includes:
-
Individuals who frequently engage in outdoor activities, like hunting, gardening, and landscaping
-
Workers in the agricultural industry who may be exposed to contaminated soil
-
People living in areas in the United States where the disease is prevalent, like California
If you fall into any of these groups, take preventative measures — such as wearing protective gear outside — to reduce your risk of infection.
Treatments for Tularemia
Tularemia is a serious bacterial infection that requires prompt treatment to prevent severe complications.
Antibiotics
Antibiotic therapy is the first-line treatment for tularemia and should be started as soon as a diagnosis is suspected. Your doctor will likely recommend the following antibiotics:
Streptomycin and gentamicin: These aminoglycoside antibiotics are considered the primary drug for treating tularemia due to their efficacy in killing Francisella tularensis. Treatment usually lasts 7 to 10 days and is typically administered intravenously.
Doxycycline and ciprofloxacin: These antibiotics are effective alternatives for streptomycin and gentamicin — especially for patients with an intolerance to aminoglycosides. They are also recommended for children and pregnant women as safer options. The treatment duration may be longer — typically 14 to 21 days — and these drugs are taken orally.
Long-term treatment
In certain cases — especially those involving severe or complicated tularemia — longer courses of antibiotics may be necessary.
Long-term antibiotic use isn’t normally recommended due to a lack of research on potential side effects and risks.
However, if you do require long-term antibiotic treatment, consult your doctor about the risks and how you can manage them.
Be sure to schedule regular follow-ups with your healthcare provider to monitor the effectiveness of the treatment and adjust it if necessary.
This may include repeated laboratory tests to ensure that the infection is responding to the antibiotics.
Can Tularemia Be Prevented?
While not all cases of tularemia can be prevented, there are a number of things you can do to reduce your risk of infection. This includes:
Wearing gloves and protective clothing when handling wild animals or their carcasses
Discouraging children from touching sick or dead animals
Using insect repellent that contains ingredients like DEET, picaridin, or IR3535
Wearing long sleeves and pants when moving through grassy or wooded areas
Mowing and landscaping with caution
Performing regular and thorough tick checks
Using proper filtration and chemical treatments when drinking untreated water
Carefully disposing of any dead animals brought into your home by pets
These strategies can help you stay informed and proactive about tularemia, thereby reducing your risk of contracting the disease.
When Should You See a Doctor About Tularemia?
If you suspect that you have tularemia, consult your doctor as soon as possible.
This disease can have serious health consequences if left undiagnosed or untreated, including:
Pneumonia
Osteomyelitis (bone infection)
Pericarditis (inflammation of the heart lining)
Meningitis (inflammation of the brain and spinal cord membranes)
Extensive tissue damage
You should schedule an appointment with your doctor if you experience any of the following:
Potential exposure to infected animals
Recent tick bites
Engaging in activities that disturb soil in areas where tularemia is prevalent
Drinking untreated water from natural sources
Developing sudden fever, chills, and intense headaches
Developing ulcers at the site of an insect bite or animal scratch
Swollen or painful lymph nodes
Eye irritation
Respiratory symptoms
Any sign of severe infection
You should also see a doctor if you suspect a tularemia infection and you are immune-compromised, pregnant, or have children.
If your symptoms persist or worsen after seeing a doctor, it’s crucial to seek further medical evaluation.
Tularemia can progress quickly, and complications can be severe without prompt treatment.
Where Can You Learn More About Tularemia?
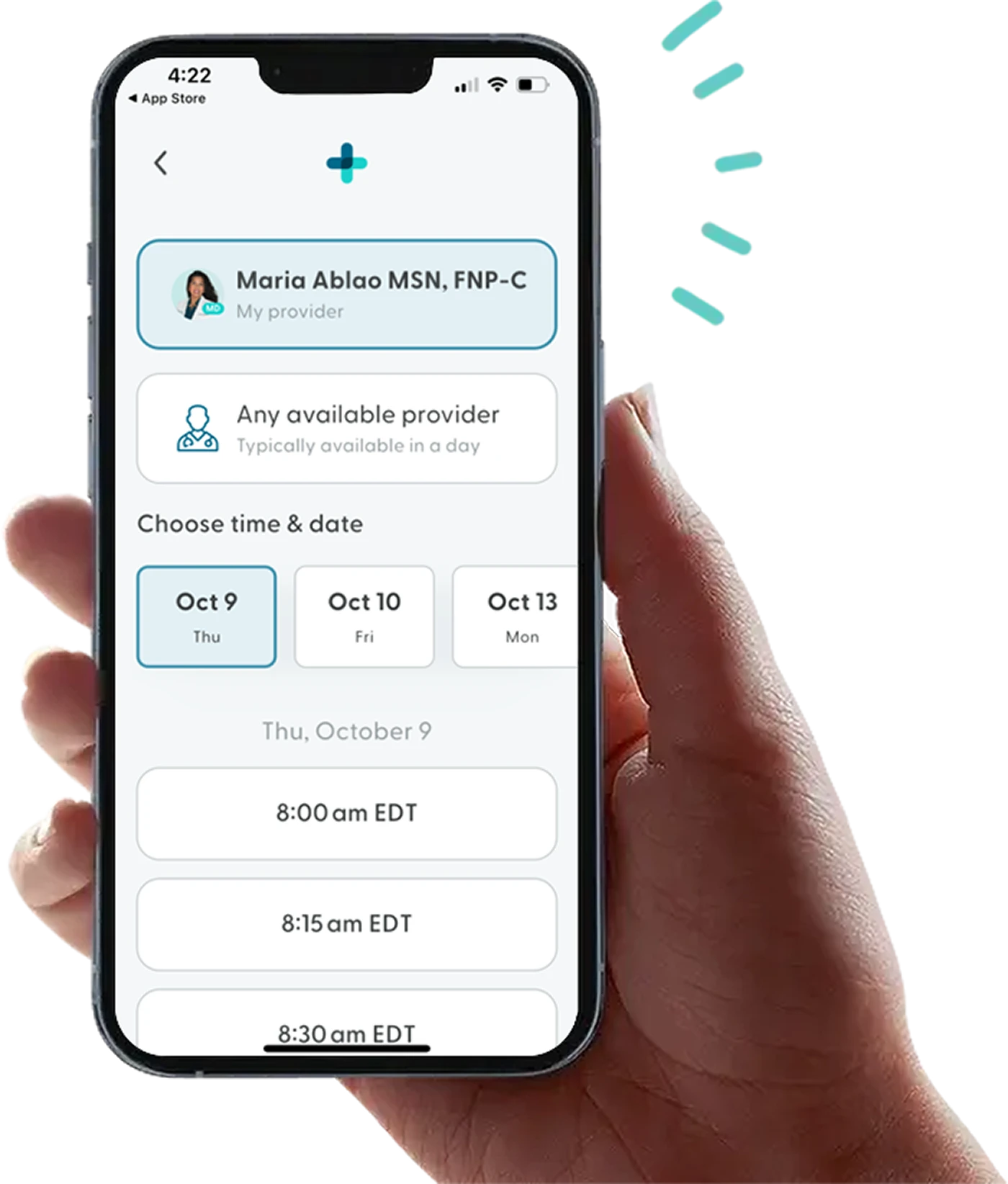
While LifeMD doesn’t provide medical care for tularemia, we can help you manage any unpleasant symptoms you may be experiencing.
A team of medical professionals can assist you with medications, prescriptions, and advice to cope with painful or uncomfortable symptoms caused by an infected tick bite.
Make your appointment today to take control of your health — all from the comfort of your own home.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.