What to Know About Postmenopausal Atrophic Vaginitis
As women get older, it's natural for their hormones to shift. Atrophic vaginitis, also known as vaginal atrophy, occurs when there is a significant decline in estrogen levels. Low estrogen levels during menopause can lead to vaginal discomfort from an increase in dryness and inflammation.
Atrophic vaginitis happens gradually, so you may not notice any symptoms right away. Some women may experience it for other reasons outside of menopause. Still, you can start menopausal treatment early to reduce the chances of developing severe symptoms. Hormone replacement therapy, OTC medications, and more can help you continue to feel like yourself as your body experiences changes and hormones fluctuate.
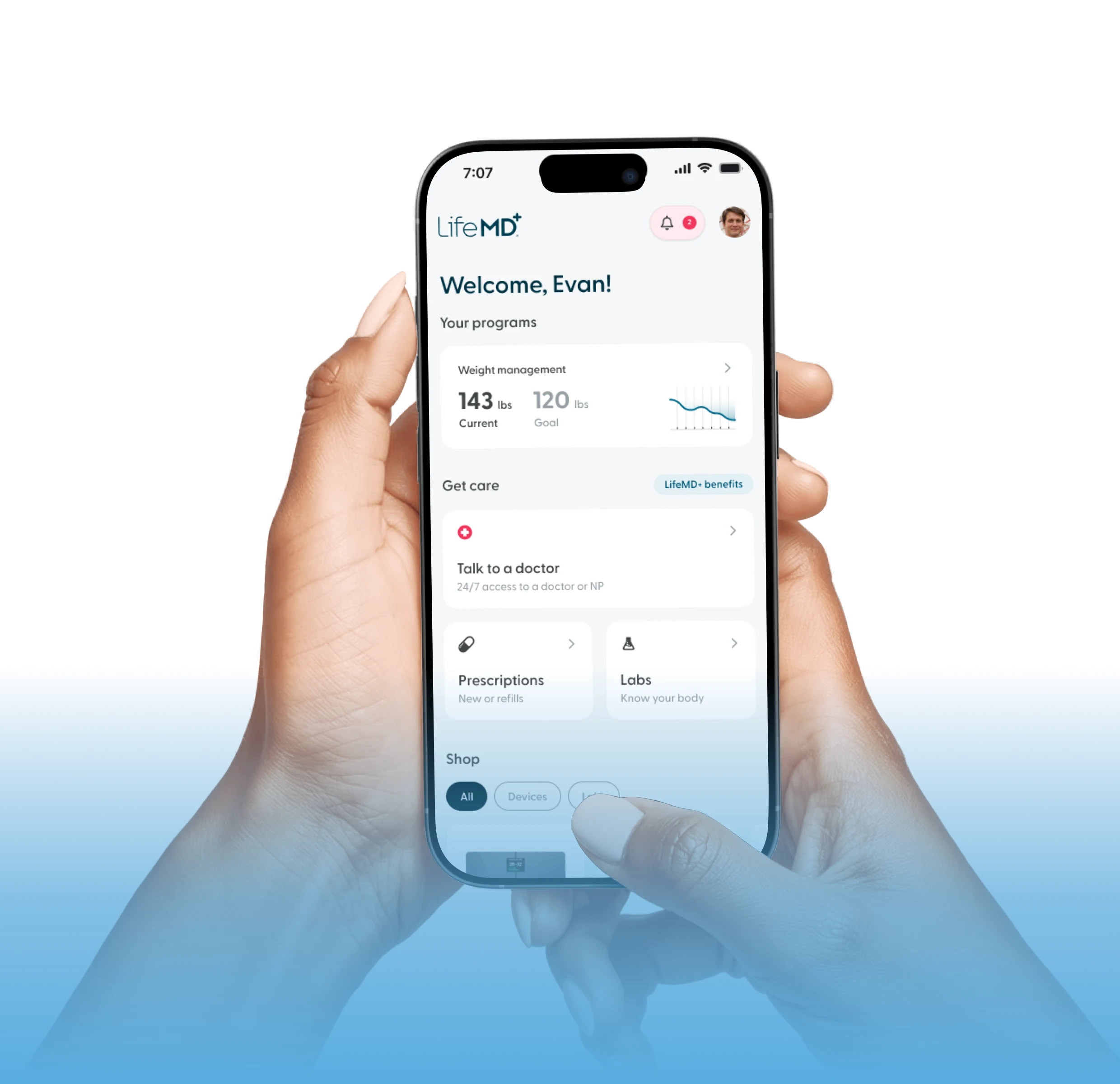
Feel like yourself again
A licensed provider can help you understand your symptoms and determine if hormone replacement therapy is the right next step.


What are the Symptoms of Postmenopausal Atrophic Vaginitis?
Women who experience atrophic vaginitis may experience the following symptoms:
Pain during sexual intercourse
Burning
Light bleeding while having sex
Vaginal itching
Thick vaginal discharge
Urinating frequently
The duration of symptoms may vary for every woman. Nevertheless, don’t hesitate to reach out to a healthcare provider as soon as you notice symptoms. Some atrophic vaginitis symptoms resemble other sexual health concerns. Incorrectly treating atrophic vaginitis or other similar symptoms may cause symptoms to linger for longer or worsen.
What Causes Postmenopausal Atrophic Vaginitis?
As women get older and move into perimenopause and menopause, the number of ovarian follicles declines and ovulation becomes less frequent, eventually stopping altogether. Falling estrogen levels lead to thinning and drying of the vaginal tissues and changes in the vaginal microbiome and pH. These changes can result in atrophic vaginitis (now often called genitourinary syndrome of menopause), which may cause dryness, irritation, and pain with sex.
Breastfeeding, certain oral contraceptives, surgery, and some medications can contribute to atrophic vaginitis, as well.
How is Atrophic Vaginitis Diagnosed?
A healthcare provider specializing in women’s health (gynecologist) can perform a physical exam to determine if you have atrophic vaginitis. If you have vaginal discharge as a result of atrophic vaginitis, a healthcare provider may also swab the inside of the vaginal wall to analyze the sample.
Who is at Risk for Postmenopausal Atrophic Vaginitis?
Atrophic vaginitis (now often grouped under genitourinary syndrome of menopause, or GSM) most commonly affects postmenopausal women, including those who experience menopause earlier than usual. Early menopause is generally defined as menopause before age 45, and premature menopause or primary ovarian insufficiency occurs before age 40.
The risk of atrophic changes is higher in women who have reduced estrogen levels, such as those with surgical menopause (removal of the ovaries), certain types of amenorrhea, or during breastfeeding, when estrogen levels are naturally lower.
Some pelvic surgeries – especially hysterectomy – may also be associated with an earlier decline in estrogen, even when the ovaries are preserved. This drop in estrogen can lead to vaginal dryness, thinning, and increased susceptibility to irritation and pain with sex.
Treatments Options for Atrophic Vaginitis
Many women may not initially seek treatment for atrophic vaginitis because of how normalized it is to be uncomfortable during menopause. However, it’s still important for your mental and physical health to feel comfortable even when you’re going through menopause.
For mild cases of atrophic vaginitis, over-the-counter (OTC) vaginal lubricants and moisturizers may help with short-term relief. For some women, engaging in sexual activity may help to improve symptoms from natural lubrication of the vaginal walls. If symptoms persist or worsen, meet with a healthcare provider to discuss options for prescription medications.
OTC moisturizers: If dryness or irritation only happens when you’re engaging in sexual intercourse, applying water-based lubricant to the surface of the vagina may relieve discomfort. Some water-based lubricants, like Replens, can last for three days.
Vaginal lubricants: Along with a moisturizer, you can use a water-based vaginal lubricant during intercourse to reduce dryness. Be careful when using lubricants with different scents. Lubricants with fragrances may increase irritation.
Hormone replacement therapy: Transdermal or vaginal estrogen can help balance vaginal pH levels and protect vaginal walls from dryness. Estrogen can help thicken vaginal walls and increase beneficial bacteria. While any form of HRT can help, low-dose vaginal estrogen is a more direct, local treatment.
Prescription medications: Non-hormonal oral medications can help reduce vaginal dryness and irritation. Local vaginal estrogen is generally considered more effective (and faster) than ospemifene for classic vaginal dryness and pain with sex. Please note that this medication may not be safe for those with a history of breast cancer.
Tips for Preventing Atrophic Vaginitis
You can’t completely prevent the hormonal changes that lead to vaginal atrophy, but you can take steps to reduce or delay symptoms – such as vaginal dryness – and help protect the health of the vaginal tissues.
Consider the following tips for managing vaginal dryness:
Consume vitamin D-rich foods or supplements
Apply natural oils to the outside of the vagina
Drink an adequate amount of water daily
Taking probiotics may help balance healthy bacteria
While these tips may help, it’s best to get treatment from a licensed healthcare provider. The source of the vaginal dryness can change what works best for you.
How to Talk to a Healthcare Provider About Atrophic Vaginitis
It can be difficult to talk to a healthcare provider about health issues affecting your sexual health. However, the sooner you have the conversation, the quicker you can find relief. Make sure to emphasize how the symptoms are affecting you in your daily life.
If you’re uncomfortable starting the conversation, consider giving your healthcare provider a written list of the symptoms you have been experiencing at the beginning of your appointment. Telehealth platforms like LifeMD also give you the opportunity to speak with healthcare providers from the comfort of your home or through messaging.
Where Can I Learn More About Atrophic Vaginitis?
Atrophic vaginitis is one of many common menopausal symptoms. At LifeMD, a licensed healthcare provider can help you navigate menopause and prescribe treatment for those who qualify.
For women approaching or experiencing menopause, the LifeMD Women’s Health Program offers treatment for menopause and other common women’s health concerns. With LifeMD, you can receive medical guidance from licensed healthcare professionals and access quality HRT, if you qualify.
Make an appointment today to get closer to better health.