Why Does My Vagina Hurt During Sex? 13 Causes of Painful Intercourse
While sex should be a time of pleasure and intimacy, for many women, it can become uncomfortable and painful.
Instead of feeling close to your partner, you may find yourself tensing up and bracing for the pain you know is coming.
This pain isn’t just physical; it takes an emotional toll as well, leaving you feeling anxious, frustrated, and even fearful of intimacy.
If you’re wondering why you’re experiencing pain during sex, you’re not alone. Painful sexual intercourse affects approximately 10 to 20% of women in the U.S.
In this article, we’ll explore the common causes of vaginal pain during sex and what you can do to reclaim your confidence and comfort in the bedroom.


What is Dyspareunia?
Dyspareunia is a medical term for persistent or recurrent pain experienced during or after sexual intercourse.
This condition can affect women of all ages and can be triggered by a variety of physical and psychological factors.
The pain can be felt in different regions of the body, including the vagina, vulva, or deep within the pelvis.
The symptoms of dyspareunia include:
A sharp pain during penetration
Deep pain during thrusting
Throbbing or aching of the vagina and pelvis after sex
Pelvic cramping
Muscle tightness or spasms
Bladder pain
The Different Types of Dyspareunia
There are three main types of dyspareunia that women may experience:
Entry pain
This type of sexual pain is felt at the entrance of the vagina during initial penetration. Causes of entry pain can include vaginal dryness, infection, and hormonal changes.
Positional pain
Positional pain is when sexual intercourse is painful in certain positions, and it’s usually related to a woman's pelvic floor muscles, vaginal dryness, or infection.
Deep pain
Also known as collision dyspareunia, this pain occurs during deep penetration.
It may feel worse in certain sexual positions and can be linked to bladder issues, bowel conditions, or pelvic floor dysfunction.
What Causes Painful Sex for Women?
There are several reasons why women may experience genital pain during sexual intercourse:
Medical conditions
Certain medical conditions, especially those that affect nearby organs and other parts of the body, can cause painful sex.
Endometriosis
This condition occurs when tissue similar to the uterine lining spreads to other parts of the reproductive system. The abnormal tissue growth causes chronic inflammation in the pelvic area, which can make pelvic tissue more sensitive to pain during sex.
Skin disorders
Skin disorders such as dermatitis cause the skin to become red, swollen, and irritated.
In the genital area, where the skin is particularly sensitive, this inflammation can lead to significant discomfort.
During sex, the friction between the inflamed skin and your partner’s body — or clothing and condoms — can exacerbate the irritation, leading to painful intercourse.
Pelvic floor dysfunction
Pelvic floor dysfunction refers to a group of conditions that affect the muscles, ligaments, and connective tissues that support the bladder, uterus, vagina, and rectum. When these muscles don’t coordinate or relax properly, they can contribute to pain, urinary or bowel symptoms, and sexual dysfunction.
When the pelvic floor muscles are too tight or in a constant state of contraction – called a hypertonic pelvic floor – penetration can become difficult and painful. The tissues around the vagina may not relax or stretch as they should, which increases friction and pressure on nerves and surrounding structures.
During or after sex, these overactive muscles can spasm or clamp down, leading to sharp, stabbing, or burning pain at the vaginal opening or deeper in the pelvis. Over time, the body can start to anticipate pain, causing even more unconscious tightening before or during intimacy, which reinforces a pain-spasm-pain cycle and can make sex increasingly uncomfortable or anxiety-provoking.
Bowel problems
Conditions that cause inflammation in the bowels can make sex painful. Irritable bowel syndrome (IBS), for example, causes significant bloating and abdominal pain.
This bloating can increase pressure on the pelvic organs and may lead to pain during deep penetration.
Bladder problems
Bladder conditions such as a urinary tract infection (UTI) cause inflammation of the urethra and bladder. During sex, the movement and pressure can irritate these inflamed tissues, leading to pain and discomfort.
The irritation from a UTI may also extend to surrounding areas, including the vaginal regions, which could result in a burning or stinging sensation during sex.
Hormonal changes
Hormonal fluctuations – especially the drop in estrogen that occurs during perimenopause and menopause – can significantly affect the moisture, thickness, and elasticity of vaginal tissues. Estrogen helps keep the vaginal lining plump, flexible, and well-lubricated.
When estrogen levels decline, the vaginal walls become thinner and more fragile, and they produce less natural lubrication. This often leads to vaginal dryness, even in women who previously never had issues with comfort during sex.
With less lubrication, there is more friction during intercourse, which can cause irritation, a burning or raw sensation, and pain during or after sex. The tissue may feel tight or “stretched”, making penetration difficult and uncomfortable. Over time, this can also lead to anticipatory tension or anxiety around sex, further impacting sexual desire and overall sexual wellbeing.
Nervous system concerns
Conditions such as a pinched nerve in the back and nerve inflammation may cause pain during sex.
This is because the nerves in the back play a crucial role in sending signals to and from the pelvic region. If a nerve in the back is pinched or inflamed, it can send pain signals to the vagina, causing discomfort.
A pinched nerve in the lower back can cause referred pain that radiates to the pelvic area, including the vagina, lower abdomen, and inner thighs.
This referred pain can make sexual activity unpleasant, even if the pelvic region isn’t directly affected.
Breastfeeding
During breastfeeding, the body produces higher levels of prolactin, the hormone responsible for milk production. Elevated prolactin naturally suppresses estrogen (and often testosterone), both of which are important for vaginal health and sexual desire. Lower estrogen can lead to vaginal dryness and reduced natural lubrication, which increases friction during sex and can make intercourse feel irritating or painful.
In addition to these physical changes, hormone shifts, fatigue, stress, and the mental load of caring for a baby can all lower sexual desire, so it’s very common for breastfeeding women to notice both discomfort with sex and a decrease in libido during this season.
Vulvodynia
Around 16% of all women in the U.S. will be affected by vulvodynia at some point in their lives.
Vulvodynia is a chronic pain condition characterized by pain or discomfort of the vulva, the external part of the female genitalia. This pain is often described as burning, stinging, itching, or tenderness.
Women with vulvodynia often have heightened sensitivity in the vulvar area, and this can make even gentle touch or pressure painful.
Genitourinary syndrome of menopause (GSM)
GSM is the medical term used to describe a group of symptoms and physical changes that affect the vulva, vagina, and lower urinary tract as estrogen levels decline in perimenopause and menopause. These changes are not just “vaginal dryness” – they can involve the vagina, vulva, urethra, and bladder and may show up as dryness, burning, irritation, pain with sex, recurrent urinary tract infections, and urinary urgency or leakage.
More than 85% of women over 40 experience GSM and this condition affects the vagina, vulva, urethra, and bladder.
Due to decreased estrogen production, women may experience vaginal dryness. As discussed above, this can cause painful sex due to increased friction.
Lower estrogen levels also lead to vaginal atrophy, and this can make the vagina feel tighter and less accommodating during sex, leading to discomfort and pain, especially with deep penetration.
Vaginismus
Vaginismus is a condition characterized by involuntary muscle contractions of the pelvic floor muscles surrounding the vaginal opening, making penetration difficult, painful, or even impossible.
These spasms are beyond a woman’s control and can occur during attempts at vaginal penetration, gynecological exams, or when trying to insert a tampon.
Many women with vaginismus develop anxiety or fear around sexual activity due to the anticipation of pain. This fear can intensify muscle contractions, creating a cycle where anxiety leads to more intense spasms and greater pain during intercourse.
In some cases, past trauma, such as sexual abuse or painful medical procedures, may contribute to the development of this condition.
Trauma or injury
Having intercourse too soon after childbirth can be significantly painful for women, which is why most doctors recommend waiting at least four to six weeks after giving birth to have sex again.
This allows the body to heal and recover from issues like vaginal tears.
Injuries like a vaginal tear from childbirth or an episiotomy, a cut made in the perineum (the area of skin between the vagina and anus) to aid vaginal delivery, can also make sex painful for women.
Infection
Conditions such as yeast infections, bacterial vaginosis (BV), or sexually transmitted infections (STIs) can cause painful sex for women.
These infections cause inflammation of the vaginal tissues, which can lead to swelling, redness, and increased sensitivity.
During sex, the friction from penetration can aggravate these inflamed tissues, leading to pain or discomfort.
Take control of your sexual health today!
Don't wait. Schedule a confidential online consultation with an experienced medical professional.


What Can I Do about Painful Intercourse?
The first step to treating dyspareunia is to consult a healthcare professional.
There are many ways a doctor can treat your symptoms, but these methods depend on the cause of your vaginal pain.
For example, if pelvic floor dysfunction is causing the pain, pelvic floor physical therapy may be the treatment your healthcare provider suggests.
Some treatments for pain during intercourse due to menopause include prescription medication, estrogen creams, and vaginal rings or tablets.
Your doctor can also prescribe medications to treat pain due to infection or underlying medical conditions.
How Do I Manage Dyspareunia?
Here are a few things you can do to make sex more comfortable and avoid vaginal pain:
Lubricant: Use a water or silicone-based lubricant to help with vaginal dryness.
Positioning: Try different sexual positions or activities until you find ones that don’t cause you pain.
Pain relievers: Take over-the-counter (OTC) pain medications before sex.
Relaxation: Find time to relax before sex and consider trying some breathing exercises.
Ice packs: Apply an ice pack to your vulva after sexual intercourse to alleviate discomfort and pain.
Where Can I Learn More about My Sexual Health?
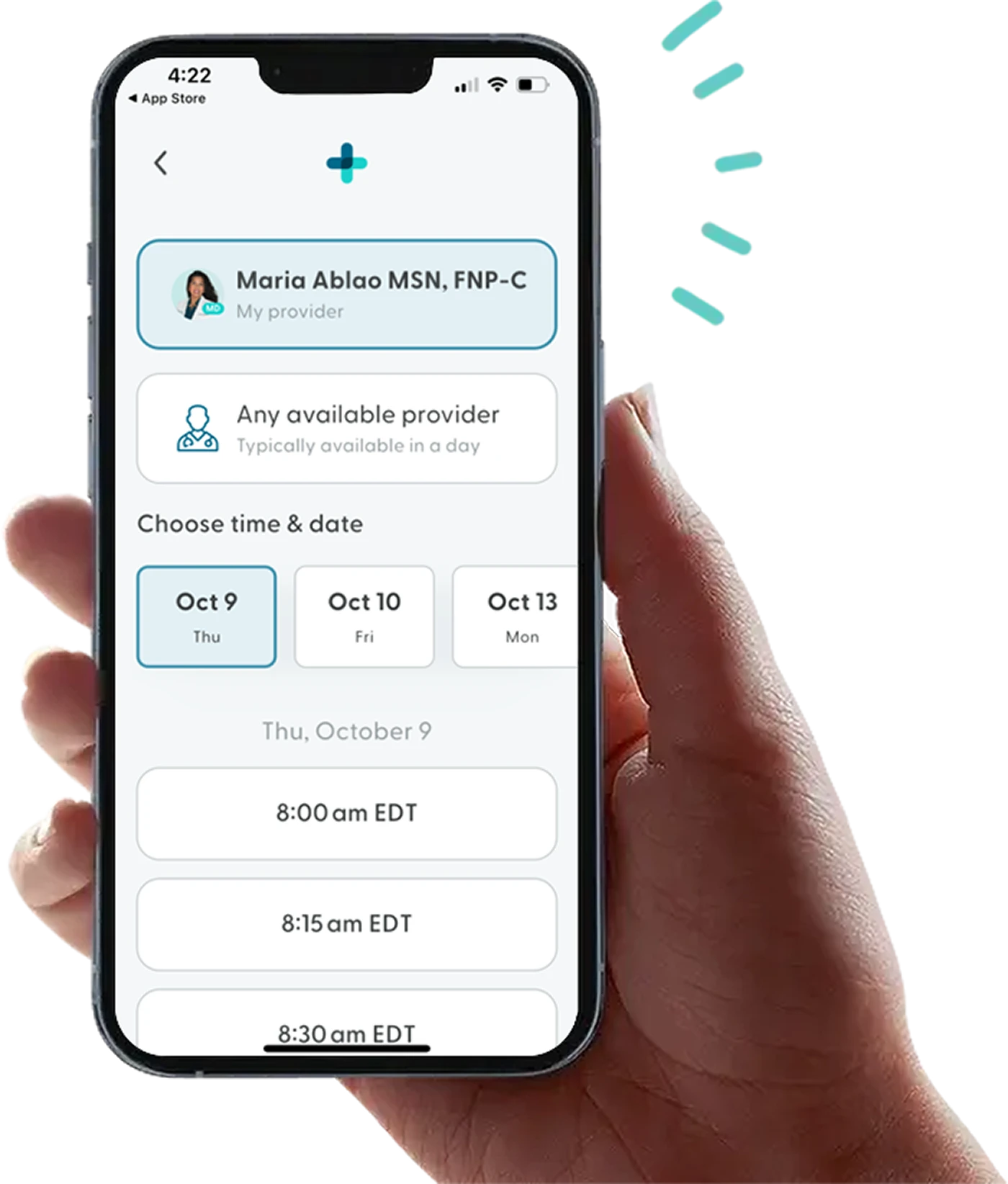
At LifeMD, you can consult a medical professional to learn more about your sexual health.
We can connect you with healthcare providers who can offer expert medical advice, treat various conditions, and order lab work.
Our consultations are conducted online through our telehealth platform, so you can get medical treatment anywhere at a time that suits you.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.
 Medically reviewed and edited by
Medically reviewed and edited by 










