How to Combat Hot Flashes in Menopause
Hot flashes are sudden waves of heat that may cause flushing, sweating, and sometimes a racing heartbeat or palpitations. While they can appear during periods, pregnancy, or postpartum, they are most common and often most disruptive during perimenopause.
Managing hot flashes depends on what’s causing them, but in menopause, women often need both immediate relief for sudden episodes and longer-term strategies to keep symptoms under control.
Why Hot Flashes Start in Perimenopause
During perimenopause and menopause, declining estrogen levels interfere with the body’s ability to regulate temperature. This hormonal shift can confuse the brain’s internal “thermostat,” leading to sudden heat surges, sweating, and flushing known as hot flashes.
Certain triggers – such as stress, caffeine, alcohol, spicy foods, or simply being in a warm environment – can make these episodes more frequent or intense.
The experience varies widely. Some women only have mild, occasional hot flashes, while others face intense and frequent episodes that interrupt sleep, affect mood, and impact quality of life.
Quick Relief for Hot Flashes
When a hot flash strikes, simple strategies can help bring immediate relief. Using a fan, sipping cold water, or wearing lightweight, layered clothing can cool the body quickly. Stepping outside for fresh air, practicing deep breathing, or using relaxation techniques may also shorten the intensity of an episode.
Avoiding common triggers – such as spicy foods, caffeine, alcohol, or high-stress situations – can make hot flashes less likely to occur in the first place.
While these approaches can be helpful in the moment, it’s important to remember they are short-term fixes. For women in perimenopause, longer-term treatments are often needed to keep symptoms under control.
Long-Term Strategies for Perimenopausal Hot Flashes
While quick fixes can help in the moment, many women in perimenopause need a more systematic, long-term approach to reduce the frequency and intensity of hot flashes.
Lifestyle approaches can make a meaningful difference. Regular exercise and maintaining a healthy weight may help regulate body temperature and improve overall well-being. Prioritizing sleep and stress reduction through practices like yoga, meditation, or breathing exercises can also lessen the impact of hot flashes. A balanced diet that limits alcohol and caffeine while keeping hydration levels up supports the body’s natural rhythm.
Medical treatments are often considered when lifestyle changes alone aren’t enough.
Hormone replacement therapy (HRT) remains the most effective treatment for moderate to severe hot flashes and night sweats. By replacing some of the estrogen your ovaries no longer make, systemic HRT helps reset the brain’s “thermostat” (in the hypothalamus), reducing how often and how intensely these temperature surges occur.
For many women, this not only eases flushing and sweating, but also improves sleep, mood, and overall quality of life. When started around the time of menopause and tailored to the individual, HRT can be a powerful tool for symptom relief while also supporting bone and metabolic health, with risks and benefits carefully weighed with a knowledgeable clinician.
Some women also find benefit from complementary approaches, including cognitive behavioral therapy (CBT), mindfulness, acupuncture, and certain supplements (though these should be used under medical supervision).
Together, these options provide a range of tools that can be tailored to each woman’s symptoms, preferences, and health needs.
Hot Flashes from Other Causes
While perimenopause is the most common reason women experience hot flashes, they can also be triggered by other medical conditions or treatments. Thyroid disorders, certain infections, cancers, or even side effects from specific medications may cause symptoms that feel similar to menopausal hot flashes.
For immediate comfort, simple cooling measures – like drinking cold water, using a fan, or practicing stress-reduction techniques – can help. However, true long-term relief depends on addressing the underlying condition with the right medical treatment.
If hot flashes occur outside of expected life stages, such as menopause or postpartum, it’s important to speak with a healthcare provider to rule out other causes and ensure the right care.
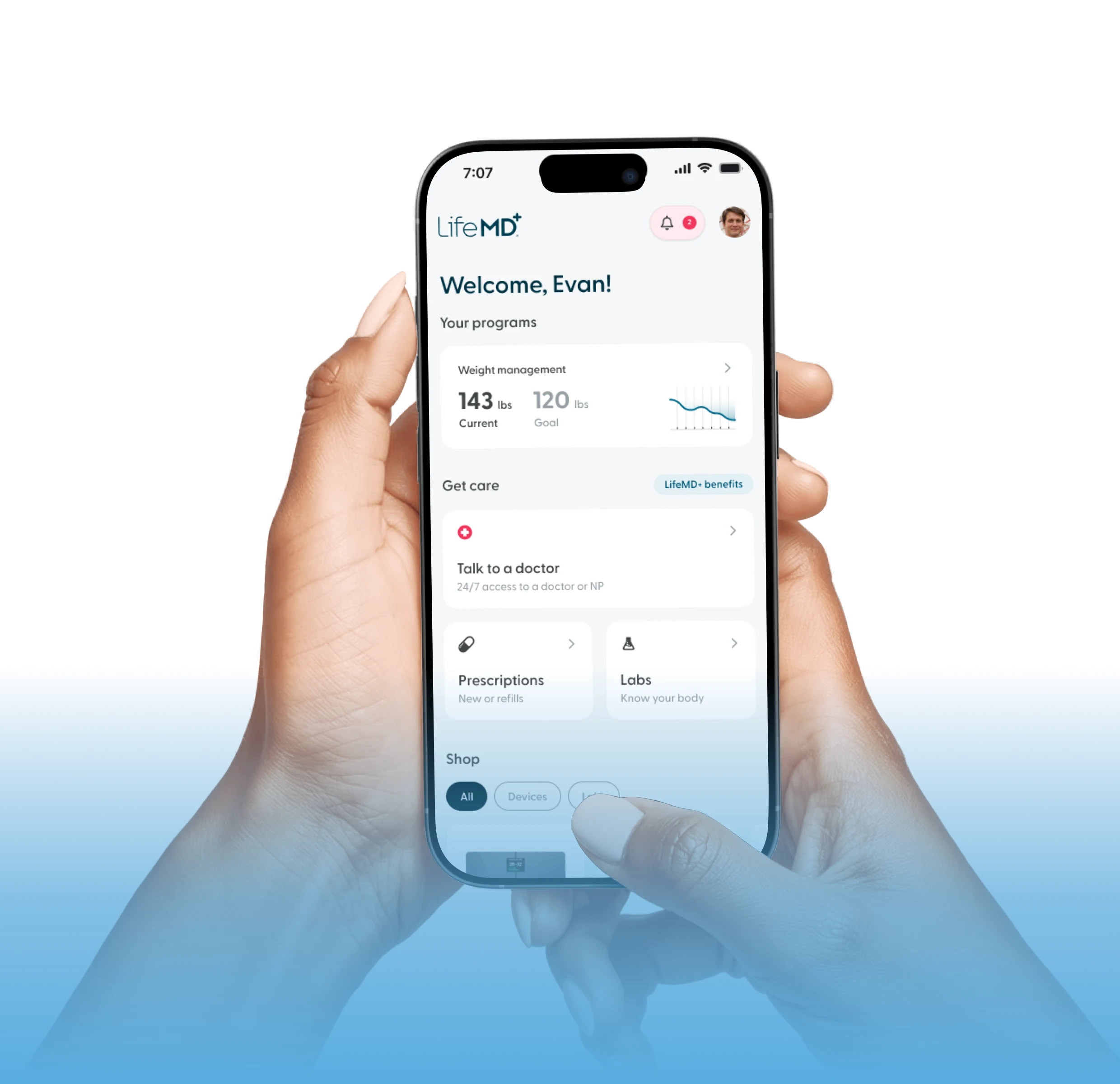
How Can LifeMD Help?
Every woman’s symptoms are different, so individualized medical guidance is essential when considering any form of HRT.
That’s why the LifeMD Women’s Health Program offers personalized care to address your hormonal imbalances and find a treatment plan that truly works for you. That means tailoring the program to your medical history and symptoms – whether it’s adjusting your dose, picking the right treatment that fits your lifestyle, or using labs to fine-tune your care.
Schedule an appointment to learn more.