Understanding Iodine Deficiency
Thyroid function plays an important role in metabolism, and iodine is one of the key nutrients the thyroid needs to work properly. Although iodine deficiency is less common in the United States than in some regions of the world, it can still occur.
Women have higher iodine needs during pregnancy and breastfeeding, which makes deficiency more likely if intake is low. Some individuals may also absorb or utilize iodine less effectively due to digestive issues, certain medications, or underlying thyroid conditions. The good news is that iodine deficiency can be identified and treated before symptoms become more severe.
What is Iodine Deficiency?
Iodine is an essential trace mineral found naturally in seawater, sea vegetables, and soil. The amount of iodine in plant foods depends on how much iodine is present in the soil, which varies by region. Some parts of the world, including Australia and areas of Europe and Asia, have low iodine levels in the soil, making deficiency more common. In the United States, iodine deficiency is less common but can still occur in people who consume little iodized salt or who have limited dietary sources such as seafood or dairy.
Iodine is required for the thyroid gland to produce thyroid hormones, thyroxine (T4) and triiodothyronine (T3). When iodine intake is too low, the thyroid cannot produce enough of these hormones, which can lead to hypothyroidism.
Because thyroid hormones regulate metabolism, low iodine levels may affect how efficiently the body produces energy. Iodine also plays a critical role in fetal brain development, which is why adequate intake during pregnancy and breastfeeding is especially important.
What is the recommended amount of iodine?
Health experts recommend that men consume around 150 mcg (micrograms) of iodine, and women need to consume 150mcg, but may require up to 290 mcg of iodine during different life stages, such as pregnancy.
What are the Symptoms of Iodine Deficiency?
Those with iodine deficiency may not always experience symptoms. Symptoms of hypothyroidism related to iodine deficiency may not manifest right away. A goiter (an enlarged thyroid) is one of the most common physical symptoms of iodine deficiency.
Those with moderate to severe iodine deficiency may also experience the following symptoms:
Constipation
Weight gain
Fatigue
Cold sensitivity
High blood pressure
Bradycardia (slow heartbeat)
Dry skin
Most of these symptoms are due to hypothyroidism. Untreated iodine deficiency can cause hypothyroidism, and hypothyroidism can also increase the risk of heart problems, depression, menstrual irregularities, and infertility.Who is at Risk for Iodine Deficiency?
Iodine deficiency is less common in the United States compared to many parts of South Asia, certain European countries, and other regions where soil iodine levels are naturally low. Environmental factors such as glaciation, flooding, and long-term soil depletion have contributed to lower iodine availability in those areas. People who follow vegetarian or vegan diets may also have an increased risk because plant-based foods generally contain lower iodine unless iodized salt or sea vegetables are consumed.
Beyond geographic and dietary factors, certain groups have an elevated risk of iodine deficiency:
• People who don’t use iodized salt • Individuals with limited dairy or seafood intake • Pregnant and breastfeeding women, whose iodine needs are higher • People with conditions that impair nutrient absorption, such as celiac disease or gastrointestinal disorders
Women who are pregnant and iodine deficient have a higher risk of complications, including impaired fetal brain development and congenital disorders. For this reason, healthcare providers often monitor iodine status more closely during pregnancy.
How is Iodine Deficiency Diagnosed?
Iodine deficiency is typically identified through a combination of clinical evaluation, detailed history taking, and thyroid function testing. During a physical exam, a healthcare provider may check for signs of an enlarged thyroid gland, called a goiter. While a goiter can occur with iodine deficiency, it does not confirm the diagnosis on its own.
There is no single test used universally to diagnose iodine deficiency in individual patients, but the following tools can help assess thyroid health and determine whether low iodine may be contributing:
Thyroid blood tests: These do not measure iodine directly, but they can show whether iodine deficiency has affected thyroid hormone production. Tests may include TSH, Free T4, Free T3, and thyroid antibodies.
Thyroid ultrasound (when indicated): An ultrasound cannot measure iodine levels, but it can detect changes in thyroid size or structure that may occur when the gland has been under strain from low iodine intake.
Urinary iodine and serum iodine tests are available, but they are not routinely used to diagnose iodine deficiency in individual patients. Urinary iodine reflects only recent iodine intake and fluctuates significantly from day to day, making it more useful for population studies than for clinical diagnosis. Serum iodine is even less reliable because it does not accurately represent the body's long-term iodine status. For these reasons, most healthcare providers rely on thyroid function tests, symptoms, and dietary patterns rather than iodine-specific lab tests.
How Can You Raise Iodine Levels?
To raise iodine levels, a healthcare provider may recommend eating more iodine-rich foods or taking iodine supplements. Let a healthcare provider know about any other supplements or medications you take before starting iodine supplements.
The following foods have high levels of iodine:
Seaweed
Eggs
Shrimp
Cod
Oysters
Dairy products
Beef liver
Iodized table salt
Key Point: Is it Possible to Consume Too Much Iodine?
Consuming too much iodine, known as iodine toxicity, can also lead to similar symptoms caused by iodine deficiency. Iodine toxicity can lead to irritation in the digestive tract or a rash. Be careful not to take more iodine supplements than recommended. In some cases, iodine toxicity can lead to hyperthyroidism.
Tips for Preventing Iodine Deficiency
The best way to prevent iodine deficiency is to continue to keep iodine-rich foods in your daily diet. Fortunately, most foods in the U.S. have naturally high levels of iodine.
The following tips can help you keep your iodine levels within a normal range:
Consider prioritizing more seafood and plant-based foods
Have at least two to three seafood meals per week
Use iodized salt while cooking
Taking iodine supplements recommended by a health professional
Limit your consumption of ultraprocessed foods
When consuming iodized salt, it’s important not to over-consume salt. Consuming too much salt for a long period of time may increase your risk of developing health conditions.
Where Can I Learn More About Iodine Deficiency?
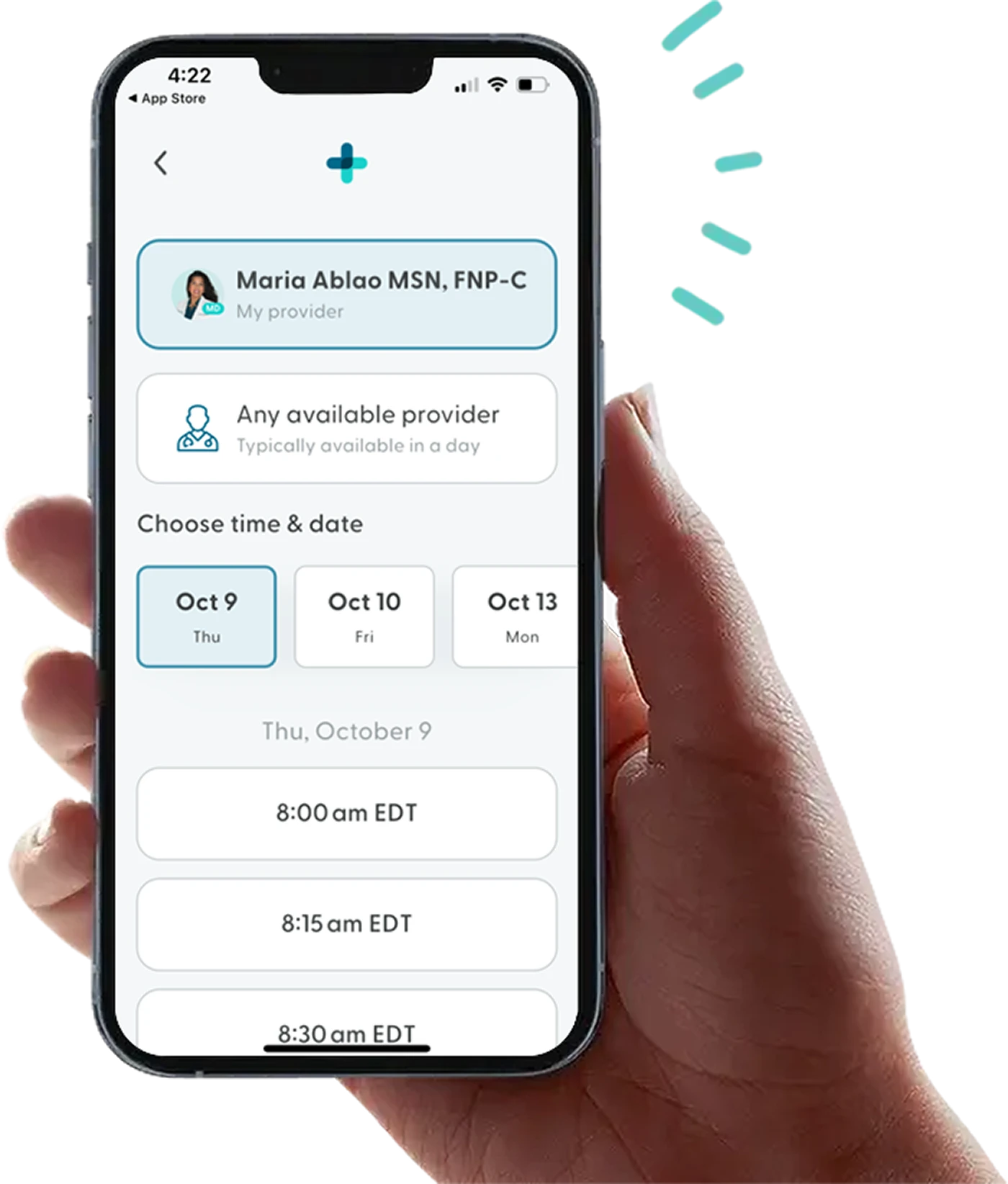
Iodine deficiency can affect other bodily functions by reducing the production of thyroid hormone. At LifeMD, a licensed healthcare provider can help you learn more about iodine deficiency and other women’s health concerns.
The LifeMD Women’s Health Program offers quality testing and lab options for thyroid treatment and other women’s health concerns. A LifeMD-affiliated healthcare provider can prescribe treatments for hypothyroidism for those who qualify.
LifeMD offers treatment for anyone needing support for thyroid complications. With LifeMD+, you can get quality testing and lab options for thyroid treatment and other health concerns related to iodine deficiency. A LifeMD-affiliated healthcare provider can also prescribe hypothyroidism and hyperthyroidism treatments for those who qualify.
Become a LifeMD+ member today to balance your hormones for an optimal health outcome.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.
 Medically reviewed and edited by
Medically reviewed and edited by 








