What is Hashimoto’s Disease?
Hashimoto’s disease is the most common cause of hypothyroidism in the United States and one of the most common autoimmune conditions worldwide. It affects the thyroid, a small butterfly-shaped gland in the neck that helps regulate metabolism, energy levels, digestion, brain function, temperature control, and overall well-being. When thyroid function slows down, it can feel as if the body’s internal thermostat has been turned too low, and everyday tasks may require more effort than usual.
Hashimoto’s occurs when the immune system mistakenly identifies thyroid tissue as harmful. Instead of protecting the thyroid, the immune system begins attacking it. Over time, this autoimmune activity decreases the thyroid’s ability to make hormones. Although Hashimoto’s is a chronic condition, it’s highly manageable. Many people feel significantly better when they understand their triggers, receive the right testing, support gut and immune health, balance blood sugar, and use appropriate medication when needed.
Why Hashimoto’s Develops
The immune system’s job is to distinguish between what belongs in the body and what does not. In Hashimoto’s, that recognition system becomes confused due to a combination of genetics and environmental triggers. Genetics create susceptibility, but they do not guarantee disease. Environmental factors, lifestyle stressors, and internal imbalances determine whether the condition becomes active.
Triggers may include gut imbalances, viral or bacterial infections, nutrient deficiencies, chronic stress, environmental toxins, hormonal transitions, and blood sugar instability. Women are affected far more often than men, likely due to the way estrogen interacts with the immune system. Many people develop Hashimoto’s during pregnancy, postpartum, or perimenopause.
Research shows that the autoimmune attack in Hashimoto’s involves both antibody production and T cell activity, leading to gradual thyroid damage.
Symptoms of Hashimoto’s Disease
Symptoms tend to develop slowly, which is why so many people go undiagnosed for years. Many patients describe feeling “not themselves” long before testing reveals the cause.
Common symptoms include:
• Fatigue or low stamina • Brain fog or memory difficulties • Weight gain or difficulty losing weight • Cold intolerance • Dry skin or hair thinning • Constipation • Joint or muscle pain • Depression or anxiety • Slowed heart rate • Irregular, long, or heavy menstrual cycles • A feeling of fullness in the throat or the presence of a goiter
Thyroid hormones affect every cell in the body, which is why symptoms may appear across multiple systems.
Important Lab Testing for Hashimoto’s and Why it Matters
A comprehensive thyroid evaluation offers far more insight than a TSH test alone. The following labs provide a complete picture of thyroid and immune function.
• Thyroid peroxidase antibodies and thyroglobulin antibodies: confirm autoimmune activity. • TSH: reflects the brain’s signal to the thyroid. • Free T4: shows how much hormone is available for conversion. • Free T3: the active hormone your cells use for energy. Many people with Hashimoto’s struggle to convert T4 into T3 effectively. • Reverse T3: identifies whether stress, inflammation, or illness is blocking conversion. • Vitamin D: essential for immune balance; low levels are common in autoimmune conditions. • Ferritin: iron storage needed for thyroid hormone production. • Zinc, selenium, and iodine status: important cofactors for hormone synthesis and antioxidant protection. • A stool test: identifies inflammation, bacterial imbalance, digestive insufficiency, parasites, and yeast overgrowth. Because most of the immune system resides in the gut, this provides key insight into autoimmune triggers. • A cortisol curve: helps identify stress patterns interfering with thyroid hormone conversion.
These tests help uncover why symptoms are occurring and which underlying factors require attention.
Root Cause Factors in Hashimoto’s Disease
Research has identified several contributors to autoimmune thyroid disease. These may act alone or interact with one another.
Gut health
Gut health plays a central role in autoimmune conditions. Approximately 70 percent of the immune system is located in the gut. When the gut becomes imbalanced, the immune system can become overstimulated.
A helpful analogy is to picture the gut lining as a tightly woven net. When inflammation, stress, infections, or poor diet irritate the gut, the holes in the net widen. Larger particles such as food proteins, toxins, or bacteria can then “leak” into the bloodstream and trigger immune activation. Over time, this may contribute to autoimmune thyroid reactions.
Research supports this connection. Studies suggest that gut microbial imbalances influence the onset and progression of hypothyroidism by affecting immune regulation, inflammation, and nutrient absorption.
Another review describes the gut–thyroid axis and notes that beneficial gut bacteria help with the absorption of selenium and zinc, minerals essential for thyroid hormone production.
A stool test helps identify gut patterns that may be driving immune activation, allowing for personalized treatment.
Nutrient deficiencies
Several nutrients play a critical role in thyroid hormone production and immune balance, and deficiencies can worsen autoimmune activity. Selenium and zinc are required for converting T4 into the active hormone T3 and for protecting thyroid tissue from oxidative stress. Iron, stored as ferritin, is needed for thyroid hormone synthesis, but excessively high iron levels can increase oxidative stress and inflammation, which may aggravate autoimmune processes. Vitamin D helps regulate immune responses and is frequently low in people with Hashimoto’s. Iodine is essential for making thyroid hormone, but both iodine deficiency and iodine excess can contribute to thyroid dysfunction.
Studies consistently show that inadequate or imbalanced intake of these nutrients correlates with higher thyroid antibody levels and altered thyroid function. that deficiencies in these nutrients correlate with higher thyroid antibody levels and worse thyroid function.
Chronic stress and cortisol imbalance
Stress plays a major role in autoimmune conditions, including Hashimoto’s. When stress levels remain high for extended periods, cortisol production can become irregular. This disrupts the conversion of T4 into active T3 and may increase reverse T3, which blocks thyroid hormone at the cellular level. Stress also weakens gut integrity and increases inflammation, both of which contribute to autoimmunity.
Patients with high stress often notice thyroid flare-ups during stressful periods. Research also shows that chronic stress alters immune regulation and can contribute to autoimmune processes.
Liver congestion and detoxification load
The liver is responsible for converting a large portion of T4 into the active hormone T3. When the liver becomes overburdened by toxins, inflammation, medications, or poor diet, this conversion process slows. As a result, thyroid hormone levels may appear “normal” on paper while patients still feel hypothyroid.
Environmental chemicals such as BPA, pesticides, and heavy metals can bind to thyroid hormone receptors or interfere with hormone production, further impairing thyroid function. Research shows that environmental endocrine disruptors have the ability to impair thyroid hormone pathways and contribute to autoimmune thyroid disease.
Gluten sensitivity and diet-related triggers
People with Hashimoto’s are more likely to have issues with gluten tolerance compared to the general population. For some, gluten may increase intestinal permeability, stimulate inflammation, or activate the immune system in a way that worsens thyroid symptoms.
Research shows that gluten removal can reduce inflammation, decrease antibody levels, and improve thyroid markers in individuals with autoimmune thyroid disease, especially where gluten-related disorders are also present. A meta-analysis found that gluten restriction improved inflammation and thyroid function markers in certain autoimmune thyroid patients.
Hormonal imbalances
Hormones have a powerful effect on the immune system, which is why women experience Hashimoto’s far more often than men. Estrogen fluctuations during pregnancy, postpartum, and perimenopause can influence immune activation and trigger autoimmune conditions. Low progesterone, insulin resistance, and adrenal hormone imbalances may also worsen thyroid symptoms. Many women first develop Hashimoto’s during hormonal transitions, which reflects the close relationship between reproductive hormones and thyroid function.
Infections and molecular mimicry
Certain viral or bacterial infections have been associated with autoimmune thyroid diseases through a mechanism known as molecular mimicry. This occurs when the immune system reacts to an infection but accidentally targets healthy thyroid tissue because the proteins look similar. Common infectious triggers may include Epstein-Barr virus (EBV), Yersinia enterocolitica, or H. pylori. These infections do not cause Hashimoto’s on their own but may activate the disease in genetically susceptible individuals.
Blood sugar instability and metabolic health
Blood sugar fluctuations place stress on the adrenal glands and thyroid. When insulin levels remain high, inflammation increases, and thyroid hormone conversion slows. Many people with Hashimoto’s notice that fatigue, cravings, and mood swings worsen when blood sugar is unstable. Stabilizing blood sugar through balanced meals, high-quality protein, healthy fats, and fiber can significantly improve symptoms. Poor metabolic health is associated with worsened thyroid hormone conversion and immune dysregulation.
Treatments for Hashimoto’s Disease
Medication often plays an important role in restoring hormone levels, but it does not correct the underlying autoimmune activity. A comprehensive approach works best, combining medication with nutrition, stress support, gut balance, and lifestyle changes.
Many patients feel better once they stabilize blood sugar, improve gut health, replenish key nutrients, reduce stress, and clean up environmental exposures. Anti-inflammatory dietary patterns can play a beneficial role in supporting immune balance.
Some patients benefit from reducing gluten or other food sensitivities, especially if they have digestive symptoms or known reactions. Research supports that gluten restriction may help reduce inflammation and improve thyroid markers in susceptible individuals.
Supplement recommendations may include selenium, zinc, vitamin D, iron, magnesium, or omega 3 fatty acids, depending on lab results.
Sleep and circadian rhythm also play major roles. Poor sleep can impair thyroid hormone conversion, increase inflammation, and worsen fatigue. Establishing a consistent sleep schedule and nighttime routine is often a key part of recovery.
Medication Options for Hashimoto’s
Thyroid hormone replacement is often an important part of managing Hashimoto’s because it restores the hormone levels your thyroid can no longer produce sufficiently. Most medications fall into two categories. The first category contains T4 only medications, which provide the inactive form of thyroid hormone that the body must convert into T3 (such as Levothyroxine).
The second category contains a combination of both T4 and T3, which may be helpful for individuals who have difficulty converting T4 into active T3. Examples include Armour Thyroid or NP Thyroid. Some people feel best with T4 alone, while others notice a significant improvement with combination therapy. The best option depends on factors such as conversion patterns, symptoms, nutrient status, and individual response.
Where Can I Learn More About Thyroid Health?
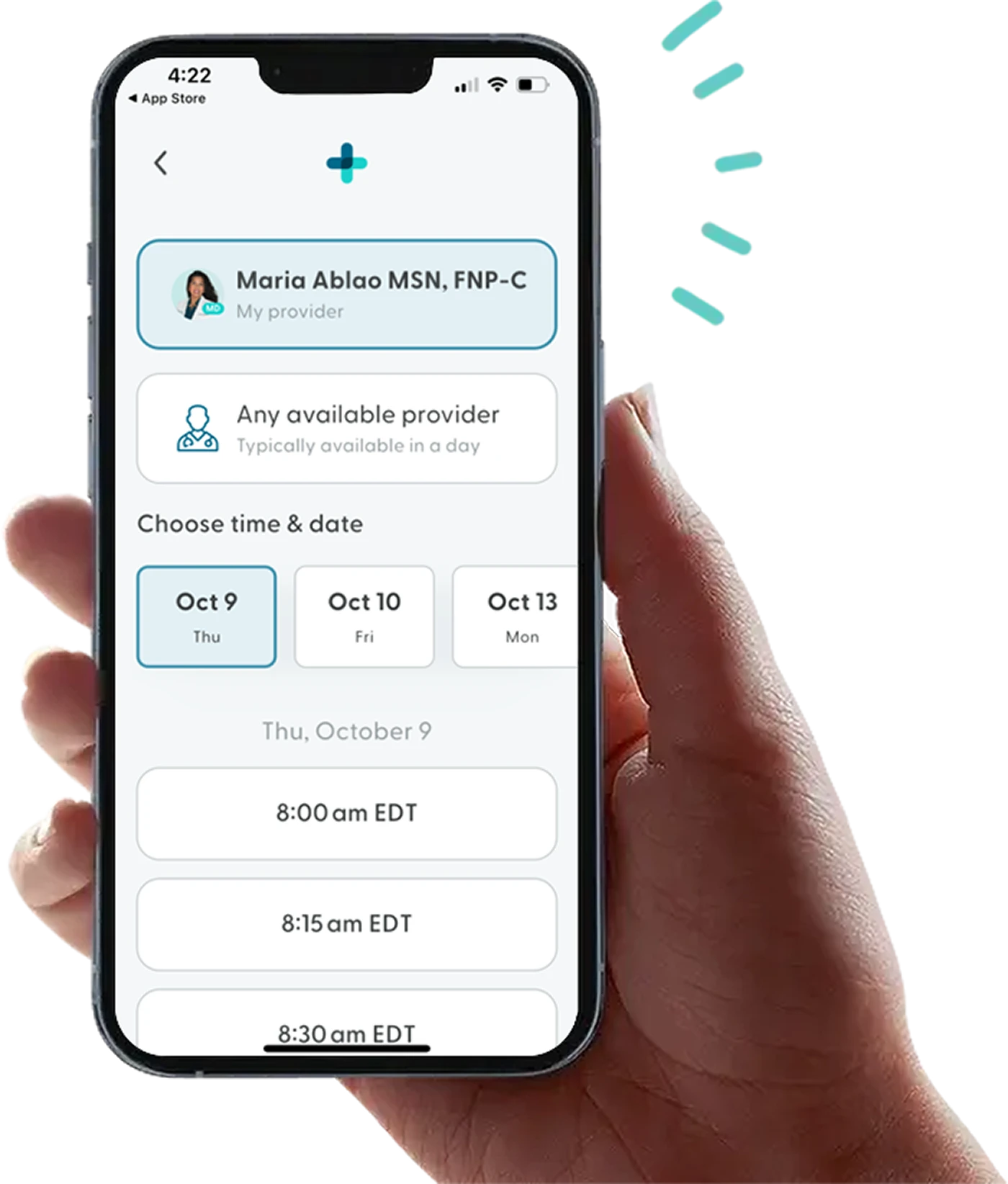
Hashimoto’s disease requires long-term management with a trusted healthcare provider. LifeMD offers treatment for anyone needing support for thyroid complications. With LifeMD+, you can get quality testing and lab options for thyroid treatment and other health concerns related to your thyroid health.
For perimenopause or postmenopausal women, the LifeMD Women’s Health Program offers quality testing and lab options for thyroid conditions like Hashimoto’s disease. A LifeMD-affiliated healthcare provider can prescribe treatments for hypothyroidism and hyperthyroidism for those who qualify. LifeMD functional dietitians can also provide dietary support and dive into other areas of health that may be contributing to thyroid function, such as gut health and nutrient deficiencies.
Get care today to balance your hormones for an optimal health outcome.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.
 Medically reviewed and edited by
Medically reviewed and edited by 








